Usher Syndrome is a rare genetic condition that causes both hearing loss and progressive vision loss due to retinitis pigmentosa (RP). It is the most common condition that affects both hearing and sight simultaneously, accounting for around 50% of all hereditary deaf-blindness cases.
This article explores the types, causes, symptoms, diagnostic methods, treatments, and support strategies for Usher Syndrome, providing evidence-based insights for patients, families, and healthcare professionals.
What is Usher Syndrome?
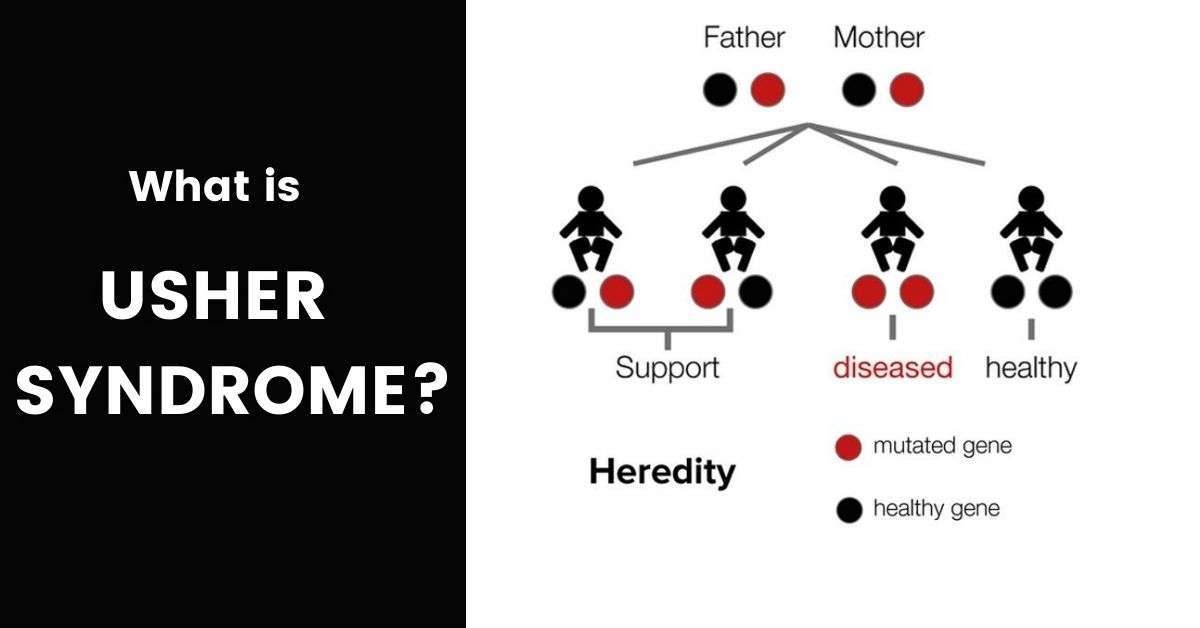
Usher Syndrome is an autosomal recessive inherited disorder, meaning that both parents must carry and pass on the defective gene for a child to develop the condition. It is characterised by:
- Sensorineural hearing loss (from birth or progressive).
- Vision loss from retinitis pigmentosa.
- In some cases, balance issues due to vestibular dysfunction.
Prevalence of Usher Syndrome
- Usher Syndrome affects an estimated 3–6% of all children who are deaf and 50% of deaf-blind individuals.
- Prevalence varies globally, but in the United States, it is estimated at 4 to 17 per 100,000 people.
- A study in Europe reported that approximately 1 in 6,000 to 1 in 10,000 people are affected.
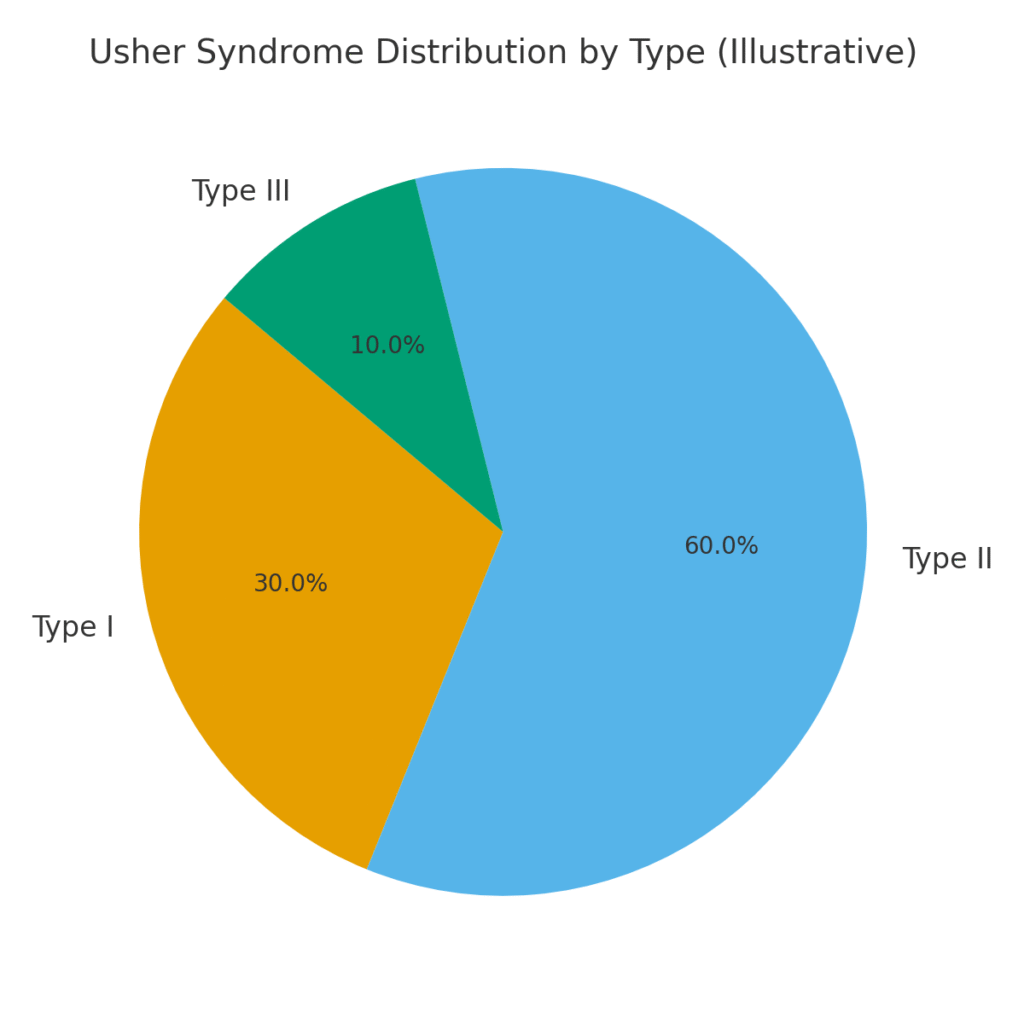
Types of Usher Syndrome
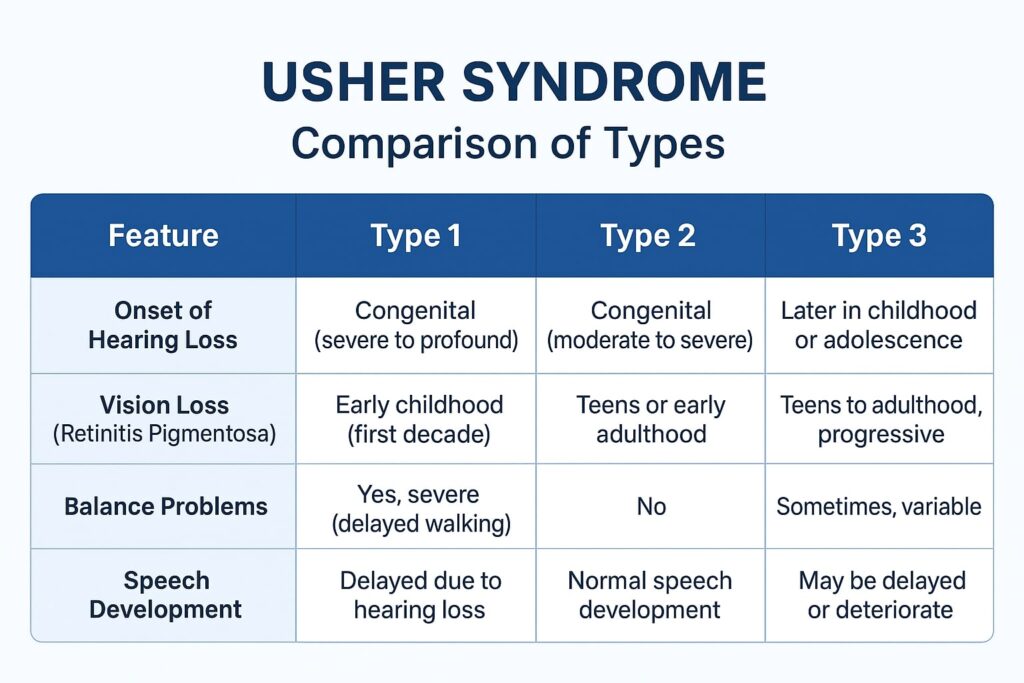
| Type | Hearing Loss | Vision Loss (RP Onset) | Balance Issues | Key Features |
|---|---|---|---|---|
| Type 1 | Profound, congenital (from birth) | Early childhood | Yes (vestibular dysfunction) | Children often delayed in walking; early blindness risk. |
| Type 2 | Moderate to severe (from birth) | Adolescence or adulthood | No | Hearing stable; vision worsens in teenage years. |
| Type 3 | Progressive (childhood → adulthood) | Teen years to adulthood | Variable | Rare; common in Finland & Ashkenazi Jewish populations. |
Symptoms of Usher Syndrome
Below are some common symptoms:
Hearing Symptoms
- Type 1 & 2: hearing impairment present from birth.
- Type 3: hearing gradually worsens over time.
Vision Symptoms
- Night blindness (difficulty seeing in dim light).
- Loss of peripheral vision (“tunnel vision”).
- Difficulty adapting to light changes.
- Progression to severe vision impairment or blindness.
Balance Symptoms
- Seen mainly in Type 1, children may struggle with sitting, standing, and walking milestones.
Causes of Usher Syndrome
Usher Syndrome is caused by mutations in at least 11 genes, including MYO7A, USH1C, CDH23, PCDH15, and USH2A. These genes are crucial for the normal development and functioning of sensory cells in the inner ear and retina.
- Inheritance pattern: autosomal recessive.
- Parents who are carriers typically have no symptoms.
- A child must inherit two copies of the faulty gene to develop Usher Syndrome.
Diagnosis of Usher Syndrome
Diagnosing Usher Syndrome involves multidisciplinary testing:
- Vestibular Function Tests: Assesses balance problems.
- Hearing Tests (Audiometry): Detects type and severity of hearing loss.
- Eye Exams: Retinal examination, visual field testing, and electroretinography (ERG).
- Genetic Testing: Confirms mutations and identifies carrier parents.
Early diagnosis is critical as intervention during childhood can significantly improve quality of life.
Treatment and Management
There is currently no cure for Usher Syndrome. Management focuses on early intervention, supportive therapies, and emerging treatments.
Hearing Interventions
- Hearing aids for mild-to-moderate cases.
- Cochlear implants in children with profound hearing loss (especially Type 1).
- Speech and language therapy.
Vision Interventions
- Low vision aids (magnifiers, screen readers).
- Orientation and mobility training.
- Vitamin A supplementation may slow progression of RP (must be medically supervised).
- Retinal implants (“bionic eyes”) are under research.
Balance Support
- Physical therapy for children with delayed motor milestones.
- Balance training and vestibular rehabilitation.
Prognosis
- Type 1: Severe, with early blindness and profound hearing loss.
- Type 2: Moderate hearing loss and vision loss starting in adolescence.
- Type 3: Variable, with gradual decline in hearing and sight.
- Supportive therapies significantly improve education, independence, and social integration.
Latest Research and Emerging Treatments
- Gene therapy trials (targeting MYO7A, USH2A mutations).
- Stem cell research for retinal regeneration.
- CRISPR gene editing shows potential but remains experimental.
- Artificial vision aids and advanced cochlear technology under development.
Living with Usher Syndrome: Patient & Family Support
- Educational support: Special schools or mainstream with support services.
- Psychological support: Counselling for patients and caregivers.
- Support groups: Organisations like Usher Syndrome Coalition provide community resources.
| Aspect | Details |
|---|---|
| Prevalence | 4–17 per 100,000 |
| Inheritance | Autosomal recessive |
| Key Symptoms | Hearing loss, retinitis pigmentosa, balance issues |
| Diagnosis | Audiometry, ERG, genetic testing |
| Management | Hearing aids, cochlear implants, low-vision aids, therapy |
| Research | Gene therapy, stem cells, CRISPR |
Quick Tips
- Get early screening if there is family history.
- Use assistive technologies (screen readers, Braille, mobility training).
- Stay connected: Join global support groups.
- Monitor eye health regularly with a retinal specialist.
Common FAQs
Here are some queries related to usher syndrome
Q1. What are the first signs of Usher Syndrome?
The earliest signs often include hearing loss from birth and night blindness in early childhood.
Q2. Can Usher Syndrome be cured?
No, there is currently no cure, but treatments such as cochlear implants, low-vision aids, and emerging gene therapies can improve quality of life.
Q3. How is Usher Syndrome inherited?
It follows an autosomal recessive pattern — a child must inherit two faulty genes (one from each parent).
Q4. What is the life expectancy of someone with Usher Syndrome?
Life expectancy is usually normal, though vision and hearing loss impact independence and quality of life.
Q5. Is Usher Syndrome rare?
Yes, affecting 1 in 6,000–10,000 people globally.
Conclusion
Usher Syndrome is a challenging condition, but early intervention, technological support, and ongoing research continue to improve the lives of those affected. With advances in gene therapy and assistive technologies, the future holds promise for better management and possibly new treatments.