In this article, we will cover all the aspects of a disease called retinopathy of prematurity (ROP). How it links to the eyes of premature and underweight babies and all other information that parents need to know.
If your newborn is premature and underweight and you are concerned about your baby’s ocular health then you are at the right place.
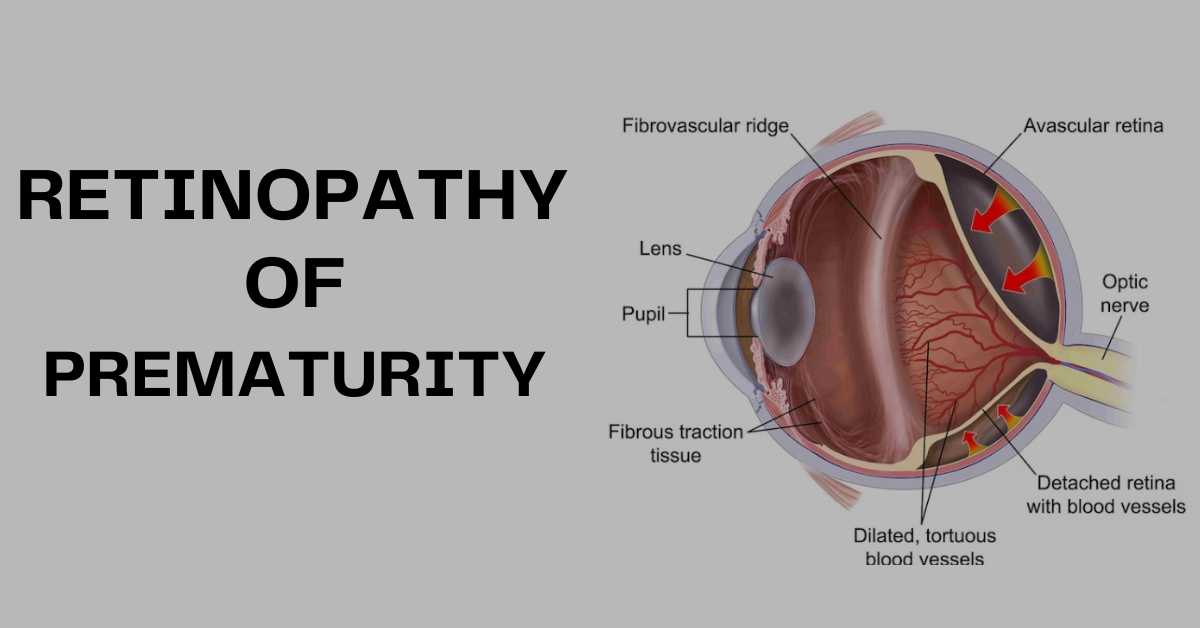
Retinopathy is simply the disease of the retina. The retina is a sensory, innermost third layer at the back of the eye. It has the potential of converting visual signals perceived by photoreceptor cells into sensory signals by ganglionic cells.
These sensory signals then are carried toward the brain. These signals end up in the primary visual cortex area of the brain which creates images.
Table of Contents
ToggleWhat is Retinopathy of Prematurity?
A disease of the retina that causes abnormal growth of blood vessels in premature babies with low birth weight is called Retinopathy of Prematurity (ROP).
A normal gestation age is about 38 to 42 weeks. In terms of months, it will be eight and a half or full nine months. If a baby is born at the gestational age of 31 weeks or less, that is to say before 7 months, the baby is called a premature baby.
Such babies are usually underdeveloped and underweight being less than 1500 g.
How does Retinopathy of Prematurity Effects Premature Children?
So what happens is, that when a baby is born premature, it is essential to place the baby in a womb-like environment. This helps in completing the baby’s development and improves his health. For this purpose premature baby is kept in incubators where supplemental oxygen is provided.
In the uterus, the fetus is present in a less oxygen environment. Whereas in the incubators, relative oxygen levels are increased. This additional oxygen often damages the developing sensitive vasculature of the retina. Vasculature refers to the blood vessels present.
What is the Pathophysiology of Retinopathy of Prematurity?
Precursor or initiator endothelial cells start the development of vessels in the retina. This happens about 14-16 weeks of gestational age.
Whereas, retinal vessels completely develop at the most posterior of the retina, between the optic disc and macula between 6 to 8 months of pregnancy.
The optic disc is the center of the optic nerve in the eye. Whereas the macula is the centermost of the retina. The macula is responsible for the best central vision.
The nasal portion of the retina develops vessels first approximately by 8 months.
Whereas in the temporal portion of the retina, vascularization (development of vessels) completes after 1 month of birth.
When central retinal vessels develop, endothelial cells migrate towards the periphery. These cells are attracted by vascular endothelial growth factor (VEGF). After that vessels start developing at the periphery too.
It is the temporal part of the retina that responds more to the disturbed oxygen supply in premature babies.
When babies are placed in an increased oxygen environment, their blood oxygen also increases. Increased blood oxygen destroy newly formed tiny vessels (called capillaries) in the temporal retina by damaging the capillary endothelium layer.
When vessels are damaged in the retina, oxygen provision decreases to the retinal cells. The retina sends a signal to the brain and the brain releases VEGF.
Vascular endothelial growth factor attracts endothelial precursor cells and initiates vascularization. This increased and abnormal development of tiny unstable vessels is called neovascularization. VEGF plays a vital role in the process of vascularization.
Is My baby at Risk of Retinopathy of Prematurity?
Following are the risk factors that may place your baby in the way of retinopathy of prematurity:
- Premature birth especially before 31 weeks of gestation
- Birth weight less than 1500 g
- High oxygen environment at birth
- Fluctuating oxygen levels
- Poor growth postnatalIncreased oxidative stress
What are the Clinical Features of Retinopathy of Prematurity?
As far as the symptoms are concerned, since the baby is way too young he demonstrates no symptoms. The only way of knowing whether the baby is developing ROP or not is by eye exam under the supervision of an eye specialist.
But the fundus (back of the eye) reveals many signs that help in understanding the zone and stage of retinopathy of prematurity.
What are the Stages of Retinopathy of Prematurity?
The fundus of the eye is examined by indirect ophthalmoscopy in premature infants. At the junction of the posterior retina with vascularization and peripheral avascular (without vessels) retina, the abnormal vascular response may be seen according to the following stages:
Stage 1:
The most highlighted feature of stage 1 of retinopathy of prematurity is the demarcation line. It is seen as the flat line of white color that distinguishes the normally vascularized retina (posteriorly) and peripheral retina with no vasculature (anteriorly).
Stage 2:
Elevated ridge is the recognizing feature of this stage. An elevated ridge, pink in appearance starts developing in the area of the demarcation line. It is present above the plane of the retina. It represents a mesenchymal shunt.
Arterioles and venules join at this point. Blood vessels start entering the ridge. Small individual neovascular tufts may be present posterior to the ridge.
Stage 3:
Stage 3 is the stage of extra-retinal fibrovascular neovascularization. In this stage, newly formed vessels extend into the vitreous cavity from the ridge. These newly formed vessels are leaky leading to vitreous and retinal hemorrhage.
Stage 4:
Stage 4 is divided into stage 4A and stage 4B. Due to the neovascularization into the vitreous cavity, the retina is pulled forwards. This results in the retina detaching from the underlying structures.
In stage 4A, partial retinal detachment is seen but the macula is not involved. Whereas, in stage 4B, partial retinal detachment occurs with macular involvement.
Retinal detachment may be exudative (due to fluid accumulation) or tractional (due to retinal pull towards the vitreous).
Stage 5:
The partial retinal detachment that existed in stage 4, progresses to total retinal detachment in stage 5. It occurs due to progressive fibrovascular proliferation. According to the recent classification of retinopathy of prematurity, stage 5 should further be divided into 3 stages:
- Stage 5A: when the ophthalmoscopy is performed optic disc is still visible
- Stage 5B: Due to retrolental fibrovascular tissue, the optic disc is not visible. This means the retina is detached from the optic disc too.
- Stage 5C: Fundus appearance of stage 5B along with anterior segment malfunctions like lens displacement, shallowing of the anterior chamber, etc.
This stage in retinopathy of prematurity is reached when the infant is 10 weeks old after birth.
Management of Retinopathy of prematurity
The most important point of managing retinopathy of prematurity is to keep track of the disease. Once the vision of the child is lost in ROP, it cannot be restored.
For this purpose vision screening is vital. What happens in vision screening is, that you take your child to the optometrist or ophthalmologist on the scheduled dates. The doctor will access the child’s vision status every time.
Premature infants with a gestational age less than 30-32 weeks with body weight less than 1500 g, being kept for oxygen therapy should undergo vision screening immediately. An ideal time for beginning screening is 4-6 weeks postnatal.
Indirect ophthalmoscopy is a technique used to view the full insides of the eye. Pupils are dilated and the doctor will check the infant’s fundus with an extra focusing/magnifying lens.
Treatment Guidelines for Retinopathy of Prematurity
There are two treatment guidelines that your eye doctor will follow after examining the infant’s eye status.
Type 1:
The following stages and conditions in retinopathy of prematurity require treatment within 72 hours:
- ROP in zone 1 with plus disease
- Stage 3 ROP within zone 1
- Stage 2 or 3 ROP with plus disease
Type 2:
In the following stages, the disease is observed only. This is because some stages of retinopathy of prematurity self-heal.
- Stage 1 or 2 ROP in zone 1 without plus disease
- Stage 3 of ROP in zone 2 but without the plus disease.
Treatment Options in Retinopathy of Prematurity
Early and mild stages of retinopathy of prematurity will resolve by themselves. With continued screening, the progression of the disease is tracked. According to the condition of the eye, your doctor might choose any of the following treatment options.
Medical Treatment
Medicines called anti-VEGF are injected into the eye. The purpose of these medicines is to stop the production of VEGF which is causing new and leaky blood vessels to form. Medical treatment is the latest and shows promising results. But this therapy will create no positive effect in the severe stage of the retinopathy of prematurity.
Anti-VEGF like Avastin (bevacizumab) is injected into the vitreous (jelly-like transparent part of the eye). From there, the drug will diffuse all around and penetrate the retina to stop the growth of abnormal blood vessels.
Laser Treatment
The choice of laser treatment depends upon your eye doctor. Mostly, this procedure has opted in the third stage of ROP. A laser ablation procedure is done to remove or burn away the peripheral retina. The peripheral retina is avascular and we have read above that this part is mostly damaged in retinopathy of prematurity.
What your doctor will do is, he will burn away the edges of the retina. The abnormal blood vessels that are growing in that part will coagulate. This will stop the progression of the disease. Ablation means surgical removal. This might damage the vision of the infant from the peripheral retina. But, the baby’s central vision can be protected.
Cryotherapy
Unlike the laser treatment, in which the specific wavelength and energy of the laser burn away the target area. In cryotherapy, a cold freezing probe is used to seal leaking blood vessels after neovascularization. This was the first safe and the most effective surgical treatment for the retinopathy of prematurity.
Surgery for the Retinal Detachment
This treatment option is for the most severe stage of the retinopathy of prematurity. When the retina is detached from the rest of the eye either partially or totally, it needs to be placed back. For this different surgical procedures are of choice. What procedure your eye doctor will choose depends upon the condition of the detached retina.
Vitrectomy is the surgical procedure of removing vitreous from the eye. Vitreous is the gel-like fluid in the eye. It maintains the volume of the eye. When the vitreous is removed, the space is filled with either saline, silicone oil, or gas tamponade. Any of the options will do the same thing. They will push back the retina towards its original place.
Scleral buckling is done by placing a band around the sclera. The sclera is the outermost whitish layer of the eye. This band will support the detached retina. Once the retina gets back to its original place, it will start growing normally again.
What is the Grading of Retinopathy of Prematurity According to Location?
For understanding the level of retinopathy of prematurity, the knowledge of zones is essential. This is because the vascularization is different in the different locations of the retina. Essentially there are three zones in ROP:
Zone 1:
The circular area at the posterior pole is centered on the optic disc. The radius of this circular zone extends from the center of the optic disc double the distance to the center of the macula. Any signs of retinopathy of prematurity in this zone indicate the severity of the disease.
Zone 2:
This zone extends from the center of the optic disc to the nasal ora serrate. Ora Serrata is the peripheral ending of the retina placed 5mm anterior to the eye’s equator.
Zone 3:
Anterior to zone 2, is the residual temporal crescent-shaped part of the retina.
What is the Active and Cicatricial phase of Retinopathy of Prematurity?
When the clinical features of retinopathy of prematurity are discussed, the stage from 1 to 3 is considered the active phase. In these stages, the retina is attached and the disease is progressing continues.
Whereas stage 4 to stage 5 is the cicatricial phase. In these phases, the retina progresses from partial to complete detachment.
What is the Plus Disease in the Retinopathy of Prematurity?
This condition is associated with a severe and advanced stage of retinopathy of prematurity. It indicates the tendency for the progression of the disease. This stage is characterized by:
- Dilated and tortuous (thick and folded) blood vessels in at least 2 quadrants (parts) of the retina.
- Vitreous haze. Vitreous haze means that vitreous is not clear when examined.
- The pupil cannot dilate.
Plus disease is diagnosed by comparison of different retinal images obtained at different levels.
What is Threshold Retinopathy of prematurity?
When along with the plus disease, stage 3 retinopathy is present in either zone 1 or 2, which is the threshold disease. It also can be a stage 3 retinopathy present in almost 8 clock hour area of the retina along with the plus disease.
What Happens if my Child can See very Less After he Grows up with Retinopathy of Prematurity?
This is the condition known as low vision. Low vision training and aids are given to the child. This will train him to the maximum to make the most out of his residual vision.
Conclusion
Retinopathy of prematurity is a major cause of childhood blindness. Researchers are still looking for the genes that may transfer this disease from one generation to the other.
But there is no doubt that some genes are involved in the production of abnormal blood vessels. On the basis of such research, ROP is placed with hereditary eye diseases.
The most important thing that as a parent you need to keep in your mind is to bring your baby for regular eye check-ups. Only in time identification of the disease can help stop its progression. The sooner the treatment starts, the more vision of the baby can be preserved. A healthy diet and good care during pregnancy are essential to prevent premature birth of the baby. Eye check-ups within 4-6 weeks of life for a premature baby are essential.

The latest research and updates straight to your inbox !
Join our subscribers for exclusive access to our monthly newsletter related to optometry

Pingback: Hereditary eye diseases that cause blindness - EyesOPT